July 2025 Safety Update: New drug for hand eczema, heart failure; warnings for testosterone meds, Opdivo; FDA halts Elevidys gene therapy; green tea drug interactions; anemia in older patients
New Drug Approval: Anzupgo for Chronic Hand Eczema
Leo Pharma’s Anzupgo (delgocitinib) cream treatment received FDA approval for treating moderate to severe chronic hand eczema. This is the first medication of its kind that is steroid-free and specifically developed for use on the hands. Chronic hand eczema is common, affecting about 10-15% of the population. The condition is characterized by painful, itchy, dry, thickened, cracked skin on the hands.
American Journal of Managed Care: "FDA Approves Delgocitinib for Moderate to Severe Hand Eczema:"
Anzupgo drug label
Read more about hand dermatitis (or hand eczema) at Dermnet.
Expanded Drug Approval: Kerendia (finerenone) for Heart Failure
Bayer’s Kerendia (finerenone) received expanded approval to treat adults with heart failure with left ventricular ejection fraction (LVEF) of ≥40%. Heart failure is a condition in which the heart is not able to pump blood to the rest of the body efficiently. Ejection fraction refers to how well your heart pumps blood: it is the percent blood pumped out of your heart’s ventricles each time it contracts.
Kerendia was originally approved in 2021 to prevent serious kidney failure and cardiac events in patients with chronic kidney disease (CKD) associated with type 2 diabetes. Now, patients need not have kidney disease and type 2 diabetes in order to take Kerendia. However, Kerendia can cause worsening of kidney function in patients with heart failure. For more, read the Kerendia revised label.
Fierce Pharma: Bayer Scores FDA Expansion for Kerendia
Read more about ejection fraction at Cleveland Clinic and heart failure at Medline Plus.
Sarepta’s Duchenne Treatment Suspended and Clinical Trials Halted Due to Patient Deaths
Update: The FDA partially lifted its ban on Elevidys, allowing treatment to resume for ambulatory patients (those with the ability to walk). These tend to be younger patients.
After initially refusing to do so, Sarepta paused distribution of its gene therapy for Duchenne muscular dystrophy (DMD) and halted clinical trials of a related drug in response to an FDA request. Two teenage patients recently died (one in March and one in June) after taking Elevidys (delandistrogene moxeparvovec), and a 51-year-old clinical trial participant died this month after taking Sarepta’s gene therapy for limb-girdle muscular dystrophy (LGMD). All three patients died from liver failure within weeks of receiving the one-dose intravenous infusion.
Duchenne, like most types of muscular dystrophy, mainly affects boys, with symptoms beginning around age four. The condition worsens over time, leading to weakness and wasting away of the body’s muscles. Elevidys was approved in 2023 under the accelerated approval pathway for four-and five year old ambulatory patients (those with ability to walk). It then received traditional approval for ambulatory patients age four and up and accelerated approval for non-ambulatory patients age four and up in 2024. This expanded approval was controversial. Last week, a committee at the European Union’s European Medicines Agency (EMA) said it was recommending against approval of Elevidys.
A journalist with a lot at stake in these developments (he has a son with Duchenne), writes about the Elevidys “showdown” and presents possible scenarios for what might happen next:
Testosterone Drugs: High Blood Pressure and Blood Clotting Warnings
In response to an FDA directive issued in February 2025, all testosterone product labels were updated this month and no longer include a boxed warning about increased risk of heart attacks and strokes. Results from a clinical trial used as the basis for removing the warning about cardiac risks, the Testosterone Replacement Therapy for Assessment of Long-term Vascular Events and Efficacy Response in Hypogonadal Men (TRAVERSE study), are also included in the update.
Testosterone products have a new warning about risk of increased blood pressure, based on required post-market ambulatory blood pressure (ABPM) studies, which confirmed a class-wide increase in blood pressure with testosterone. Testosterone is not recommended for use in men with uncontrolled hypertension; patients should monitor their blood pressure during treatment.
The drug labels also warn that cases of venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), have been reported in patients using testosterone products. Symptoms of venous thromboembolism (blood clot in the veins) may include lower limb pain, edema (swelling), erythema (skin reddening), and shortness of breath or chest pain. Patients experiencing these symptoms should discontinue the drug and seek urgent medical care.
The revised warnings affect all formulations of testosterone replacement therapy, including gels, tablets, patches, buccal (applied to upper gum or in the cheek), capsules, and injections. These medications are approved for males with conditions associated with a deficiency or absence of testosterone, which is either primary hypogonadism or hypogonadotropic hypogonadism. The condition is also referred to as “Low-T” or low testosterone.
Primary hypogonadism happens when the testes themselves do not function properly. Hypogonadotropic hypogonadism occurs there is a problem with the pituitary gland, which is the gland responsible for releasing hormones which in turn trigger the testes to release hormones. Testosterone was initially approved as a drug treatment in 1953.
Recently revised testosterone drug labels reported in the FDA’s Safety Related-Labeling Changes Database include: Azmiro (testosterone cypionate) injection, Aveed (testosterone undecanoate) injection, Androgel (testosterone) gel, Jatenzo (testosterone undecanoate) capsules, Kyzatrex (testosterone undecanoate) capsule, liquid filled. If you are taking a different testosterone replacement therapy, it will have similar label updates .
Read more about hypogonadism (low testosterone) at MedLine Plus.
Opdivo (nivolumab) Injection for Intravenous Use
Cancer drug Opdivo updated the postmarketing experiences section of its label to add that cases of tumor lysis syndrome have been reported. Considered a medical emergency, tumor lysis syndrome happens when cancer cells, released into the bloodstream as a result of cancer treatment, release toxins that can injure the kidneys. Tumor lysis syndrome may involve high uric acid, high phosphorous levels, or high potassium levels in the bloodstream. Opdivo was approved in 2014 and treats a variety of cancers.
FDA Safety Update for Opdivo and Opdivo Revised Label
Read more about Tumor Lysis Syndrome at Cleveland Clinic.
Medication Tips: Green Tea and Drug Interactions
The People’s Pharmacy’s Terry Graedon presents results from studies that examine the effect of green tea on absorption rates for some prescription drugs. For example, one study showed that green tea can lower concentrations of the beta blocker blood pressure drug nadolol (Coreg brand name), atorvastatin (Lipitor brand name) for cholesterol control, digoxin for heart failure, fexofenadine (Allegra brand name) for allergies, lisinopril for high blood pressure and osteoporosis medication raloxifene (Evista brand name).
On the other hand, green tea increased the absorption of sildenafil (brand name Viagra).
Green tea does not appear to interact with metoprolol (Lopressor brand name), another beta blocker drug. Read more tips about green tea interactions here:
“Does Green Tea Interact with Prescription Drugs?” at The People’s Pharmacy
Taking a blood thinner like warfarin (Coumadin brand name) or Plavix? Check out Cleveland Clinic’s guidance on what to avoid when taking blood thinners.
Medication Tips: Treatments for Anemia in Older Adults
Anemia is a common blood disorder affecting between 12-20% of those age 60 and up. Left untreated, it can cause symptoms like fatigue, weakness, headaches, leg cramps, feeling cold, and brain fog. In older patients, these signs are sometimes mistaken for normal aging, so the condition may not be documented within a patient’s medical record. Anemia can be triggered by a variety of conditions, including nutritional deficiencies, surgery, internal blood loss from polyps or ulcers, and chronic diseases like heart disease, kidney failure, or inflammatory bowel disease. Frustratingly, for about one-third of patients, the underlying cause cannot be explained. Sometimes the condition comes and goes, for no apparent reason.
First-line treatment for anemia is usually oral iron supplements, or sometimes vitamin B12 or folate. Iron pills can be hard to tolerate for many seniors (causing side effects like nausea or constipation) and may be ineffective. Read KFF’s report on anemia in older adults and why in some cases intravenous iron infusions may work better than oral supplements:
KFF News: “Maybe It’s Not Just Aging. Maybe It’s Anemia”
In severe cases of iron deficiency anemia, a patient may need a blood transfusion:
Medpage Today: “Everything you need to know about blood transfusions and anemia”
Thanks for reading Ask a Patient® Health News: Drugs & Treatments!
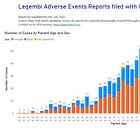
Did you miss our recent update on Leqembi, the new Alzheimer’s treatment or our June list of recalls and safety news? Check them out here:
Our website at www.askapatient.com contains a database of medication reviews and ratings contributed by patients.
Finally, if you enjoyed reading this newsletter or found it helpful, please click the ❤️ button below or at the top of the page so that more people can discover it on Substack. Thank you!